DIEP flap and autologous tissue transfer: The latest research and future developments
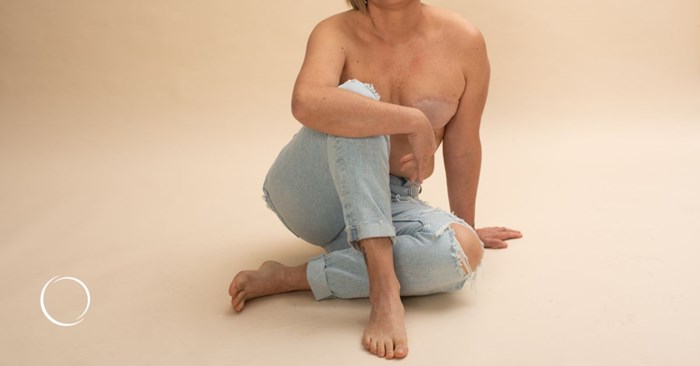
Breast cancer is a challenging diagnosis thousands of American women face each year. Many survivors hope to regain a sense of normalcy after conquering breast cancer. For most women, this involves reconstructive surgery to restore the natural appearance of their breasts after mastectomy.
If you or a loved one is considering breast reconstruction after cancer, you should know about the latest innovations. These include autologous tissue transfer techniques like deep inferior epigastric perforator flap surgery, known as DIEP flap.
Doctors developed the DIEP flap technique in the 1990s. By the 2000s, it became more common as surgeons recognized its advantages over other less gentle flap methods that use not only your fat layer but also some of your abdominal muscles.
The procedure is widely available
As DIEP flap has become more popular, more plastic surgeons than ever are performing this technique, which is more readily available now than it was in the past.
"For about 10 years, I was the only person in my state to offer the procedure. Today, there are many other surgeons who do it," said ASPS Member Surgeon Anureet Bajaj, MD.
How the DIEP flap technique works
DIEP flap reconstruction involves taking the skin, fat and blood vessels from your abdomen (similar to what's removed in a tummy tuck) and relocating them to your chest to create a new breast mound. The DIEP method leaves your abdominal muscles intact, unlike traditional flap techniques, which allows for a quicker recovery and reduction in the risk of complications.
Advanced imaging supports precision
For DIEP flap operations, many surgeons are now using advanced imaging techniques, such as magnetic resonance angiography, to map the blood vessels in the abdomen precisely. This mapping allows for greater precision during the procedure, reducing the chances of complications because the surgeon can better locate where your blood vessels are. This visual aid gives them more reliability as they dissect the flap.
"Otherwise, we're doing it blind, if you will. We're elevating our flap and looking for vessels with our eyes," said Bajaj. "Whereas if we have an MRI, we've got a map beforehand so that when we're doing surgery, we can follow the map and identify the vessels and the veins."
One of the critical aspects of the DIEP flap procedure is identifying and preserving the deep inferior epigastric perforator blood vessels. These tiny vessels provide blood flow to the transferred tissue.
Using microsurgery techniques, the surgeon connects the flap's blood vessels to those in the chest. This connection ensures the flap receives a sufficient blood supply in its new location. Surgeons use specialized instruments and sutures thinner than human hair to complete this process.
Robotics aid in surgery
The rise of robotic surgery in various medical fields also impacts DIEP flap procedures. Robots can provide greater dexterity and a steadier hand, potentially minimizing surgical trauma and improving flap survival. Yet, robotic surgery is usually not available at most plastic surgery practices.
"The robotic surgery for deep flaps is new, and mainly larger academic institutions are the best bet for that right now because I don't think that's commonplace," said Bajaj.
Postsurgical care has improved
Many surgeons are now implementing enhanced recovery after-surgery protocols, resulting in shorter hospital stays and a faster return to daily activities. They include preoperative education and physical therapy. Some patients also benefit from wearing compression garments and receiving lymphatic massage.
"I would say that that's all surgeon-specific. But all of that, combined with good nutrition and the ability to mobilize early after surgery with the new ERAS (enhanced recovery after surgery) protocols, makes a big difference for most patients," said Bajaj.
Scars are becoming thinner
The scars from DIEP flap procedures are becoming less noticeable thanks to innovations in surgical techniques and post-operative care. Newer suture materials and techniques mean less tension on the wound, leading to more aesthetically pleasing results.
"As plastic surgeons, we understand what causes scarring," said Bajaj. "A lot of times, surgeons will close the incision only at the skin layer and not the deeper layers. But plastic surgeons close incisions from the deep layers on up because that's where your strength layer is. By doing a layered closure, that alleviates tension."
Bajaj adds that other skin closure devices, such as bridges that help bring the wound edges together, alleviate tension on the incision.
The path ahead
Breast reconstruction, including DIEP flap autologous tissue transfer, has improved during the past decade. For you, as a potential patient or someone supporting a loved one, understanding the latest advancements can empower your decision-making.
The future is bright, with continuous research and developments promising even better results for breast cancer survivors. The journey from diagnosis to recovery is arduous, but with the ongoing innovations in autologous tissue transfer, the path to regaining a sense of self becomes easier and more hopeful.
To find a qualified plastic surgeon for any cosmetic or reconstructive procedure, consult a member of the American Society of Plastic Surgeons. All ASPS members are board certified by the American Board of Plastic Surgery, have completed an accredited plastic surgery training program, practice in accredited facilities and follow strict standards of safety and ethics. Find an ASPS member in your area.
