Consult Corner: Laceration through the nail bed
Editor's Note: "Consult Corner" addresses a consult commonly encountered by an on-call resident. The column begins with the reason and assesses questions that might go through a resident's mind as he or she heads to the emergency department to see the patient. Key aspects of the history and physical are discussed, as well as additional testing that should be obtained. Finally, a review of the decision-making process will present possible management strategies, all of which are synthesized into the context of an actual case.
MESSAGE ON YOUR PAGER: LACERATION THROUGH NAIL BED, CALL BACK PLEASE.
It's midnight, you're covering hand call in the pediatric E.D. - and your pager goes off. The message reads:
"4-year-old girl jammed finger in door and has a laceration through the nail bed"
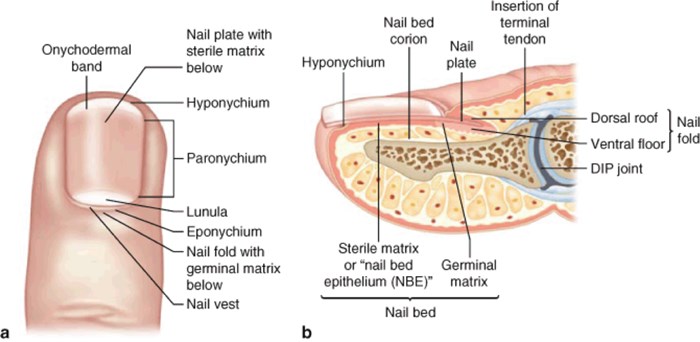
The eponychium refers to the dorsal nail fold and the skin proximal to the nail, while the hyponychium refers to the palmar skin distal to the nail. The paronychium refers to the skin around the lateral nail folds.
On the nail itself, the lunula is the white, semilunar part of the proximal portion of the nail. The nail bed lies directly underneath the nail plate. The nail bed is composed of the germinal matrix and the sterile matrix. Proximal to the lunula is the germinal matrix, which is responsible for nail growth and is located from 7-8 mm under the eponychium to the edge of the lunula. Nails grow very slowly, at a rate of 0.1 mm/day, so it will take several months for the nail to regrow. Distal to the germinal matrix is the sterile matrix which is responsible for adherence of the nail to the nail bed.
History
The timing and mechanism of injury is important to document. As with any hand injury, hand dominance and hobbies and/or occupation is important to note, if relevant, since many of these patients tend to be younger kids. Always ask about tetanus vaccination. If that's not up-to-date, they should receive a tetanus booster.
Exam
Oftentimes the nail has already been avulsed, but if not, nail-bed lacerations can be associated with subungual hematomas. If the subungual hematoma involves greater than 50 percent of the nail, the nail should be removed and the nail bed should be examined for the presence of a nail-bed laceration. Other things to note are degree of contamination and exposure of bone. All patients should have a complete hand exam.
It's important to obtain an X-ray to rule out any fractures. Nail-bed injuries are commonly associated with tuft fracture of distal phalanx. Repairing the nail-bed laceration should reduce the tuft fracture.
To Repair a Nail Bed Laceration
Lidocaine (digital block)
25-G needle, syringe
Digital tourniquet (cut off piece from glove finger)
Normal saline
Betadine
Iris scissors, periosteal elevator
6-0 fast gut or chromic suture
Stent for nail fold (part of suture packet if nail is unsuitable)
Antibiotic ointment
Procedure
You perform a digital block by injecting 1-2ml of lidocaine at the volar aspect of the proximal flexion crease of the finger (in children, always remember to verify the maximum amount of local anesthetic appropriate for the child's weight, to ensure that you do not administer more than id required). Depending on the age and cooperation of the child, you may need additional forms of sedation. Give the local anesthetic at least 5 minutes to take effect. While you are waiting, you can set-up the rest of your supplies.
Copiously irrigate the wound with at least 1 liter of irrigation. Apply a finger tourniquet to the base of the digit to aid in hemostasis. Prep the hand with Betadine, and towel appropriately. Assess the nail bed.
Repair the nail-bed laceration with dissolvable sutures (fast gut or chromic). Repair any other associated lacerations on the finger which can be done with nonabsorbable sutures for any lacerations outside of the nail bed, if the child will tolerate removal in clinic setting. If not, use absorbable sutures.
If the nail's still in place, use Iris scissors or a periosteal elevator to spread at the hyponychium. Advance proximally until the instrument reaches the nail fold - and then the nail should be able to be easily removed with a hemostat or forceps.
It's important to stent-open the eponychial fold to prevent it from scarring down, which would impair proper regrowth of the nail. To fashion a stent for the eponychial fold, you can use the foil from a suture pack or xeroform; cut into the shape of a nail; and tuck it under the fold. If the parents brought the nail in, that can be used as a stent after being properly washed in Betadine. The stent can be secured with a chromic suture in horizontal mattress fashion, with the knot on the eponychium, so that the nail is pulled under the fold by the suture. One additional, simple suture can be placed through the stent at the hyponychium to prevent the stent from flipping off of the nail bed.
Dressing
Bacitracin, Xeroform and a gauze wrap are commonly used. Beware that Xeroform can stick to the nail bed which can be very painful to remove in clinic after the dressing has been in place for a few days. Using a nonstick dressing over the Bacitracin and the laceration (such as Telfa) will help with dressing removal. For younger children, it's prudent to place a soft, bulky gauze dressing with a light Ace bandage wrap on the extremity to prevent additional trauma to the digit. If there is an associated distal tuft fracture, place finger in an extension splint. The distal interphalangeal joint should be splinted in extension. A nail-bed laceration with a tuft fracture is technically an open fracture, so these patients should be discharged on oral antibiotics as well. Follow-up in clinic in one week for a wound check.