Dear Abbe: You didn't know the patient was litigious – but here they are
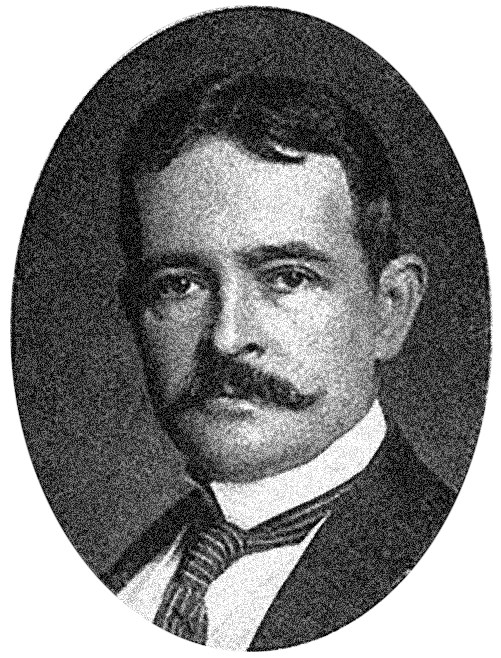
EDITOR'S NOTE: "Dear Abbe" – named in honor of plastic surgery pioneer Robert Abbe, MD – provides plastic surgery residents an opportunity to anonymously share concerns and seek advice from a highly respected, senior-level faculty member. Christian Vercler, MD, a clinical associate professor in the Section of Plastic Surgery at the University of Michigan, steps into Dr. Abbe’s shoes for this installment. The views expressed in this column are those of the author and should not be considered legal advice. Residents and Fellows are encouraged to submit questions to DearAbbe@PlasticSurgery.org. Names will be withheld.
Dear Abbe: My patient has become known for their use of the legal system to address perceived "wrongs" in their treatment. What are my options when they still need medical treatment?
– Holding my Breath
Dear Holding,
Few things induce chest pain and nausea like dealing with the legal system. Even if you're not being named in a lawsuit, having attorneys in your life can be stressful. Remember Medicolegal 101: Do not try to hide anything, do not alter any medical records and keep careful records of everything you do.
There are several reasons why patients sue surgeons, but it's most often because the patient is angry, feels wronged or lied to and wants truth and justice. You might be dealing with a litigious patient who's decided to sue you – or you may be seeing an unhappy patient who's suing someone else and you're the "second opinion."
The instinct in either situation is to distance yourself from the chaos. Unfortunately, that's not always a helpful response. Again, one of the reasons patients sue is because they feel ignored or that something's being covered up. Not being in the room and actively managing those perceptions is unnecessarily risky. When the patient has ongoing needs, you should see the patient more often rather than less; show compassion and listen to their concerns; and be transparent and honest. Avoid abandoning the patient. Don't "do a favor for the patient" and stray from the standard of care or cross professional boundaries. A friend and colleague who spent his career as chief legal counsel for my institution always advises: "Just focus on doing the right thing for the patient. I would much rather defend you after you've followed the standard of care, and not after you've done a bunch of random things you think will help in court." Don't argue with a patient in the clinical setting – most lawsuits are driven by anger, and "winning" an argument won't change how they feel.
When managing a patient who's suing someone else but still requires ongoing care, several points need to be considered. Don't join or add to their negative discourse about their prior surgeon. Although seeing a poor result from a colleague can confirm a suspicion that you are a superior surgeon, don't indulge in that conceit. Focus on setting realistic expectations for the patient's outcome going forward. Facilitate other referrals if necessary – and those referrals may need to include counseling. Suffering an adverse outcome and requiring ongoing medical care can take its toll mentally and emotionally on patients. Seeking the best interests of the patient is our professional duty.
A study performed by Austin Remington, MD, and his colleagues at the University of Michigan1 showed that poor communication, inadequate informed consent and deficient documentation were associated with malpractice claims resulting in a payment. So practice an evidence-based approach by being present to your patients and focusing on communication – and not only with the patient, but with the other clinicians involved in their care – by engaging in shared decision-making around the indications for operations and making sure the patient understands the risks. Of course, you must also document all of those discussions in the chart, as well as all your encounters and the rationale for your decisions.
Dealing with a litigious patient is stressful, so have a low threshold for seeking support for yourself. That may mean involving your own legal counsel early, talking with colleagues or seeking professional psychological support.
- Remington AC, Schaffer A, Hespe GE, Yugar CJ, Sherif R, Vercler CJ. Understanding factors associated with paid malpractice claims in plastic surgery. Plast Reconstr Surg. April 2023 [online ahead of print].